Clinical Case presentation:
First clinic visit: October 30th, 2008
CC: 5 years old male came to the clinic complaining of the puffy eye for 1 day. The patient woke up with this eye swelling yesterday. The patient denies pain, lesions, discharge, trauma or any vision changes.
Past medical history is unremarkable and immunization up to date
Initial DDX: cellulitis, blepharitis, periorbital cellulitis, chalazion or hordeolum
PE:
Vital Signs: within normal limit
Eyes: no masses, or lesion notes, swelling upper lid but non-tender to palpation. Fluorescein stain shows no foreign body presence. conjunctiva clear. Lid eversion shows no other foreign body
Heart: normal rate and rhythm, s1 and s2 are present.
Lungs: clear to auscultation bilaterally. no adventitious sound
Diagnosis: eye swelling r/o allergic reaction
Plan: warm compression, antihistamine
RTC if > pain, swelling, or visual changes
Second clinic Visit: November 1st, 2008
November 1st: child returns increase swelling, nasal congestion 2+ tenderness tissue
PE:
Temp 101.4
Eyes: Increase swelling, 2+ tenderness to tissue, EOM intact, no proptosis
DDX- cellulitis of the eye
Plan: Augmentin (Amoxicillin/clavulanic acid)
Immediate ophthalmology appointment
3rd clinic Visit: November 8th, 2008
patient return with persistent eye swelling, low-grade fever, weak and tired, knee pain with a limp.
No hx of trauma
Initial DDX: septic arthritis, cellulitis. osteomyelitis, viral syndrome (influenza, mono, CMV), Synovitis, orthopedic(SCFE, Osgood schlatter)
PE: 101.6 orally
Eye- lid still 2+ swollen, non-tender, no discharge
Skin- clear to inspection
HEENT- unremakable
Neck- positive posterior cervical LN 1 cm in size, non-tender, mobile
Heart: normal rate and rhythm, s1 and s2 are present.
Lungs: clear to auscultation bilaterally. no adventitious sound
Abdomen: bowel sound present in all four quadrants, soft, non-tender. 2 fb non-tender mass in LQU, no hepatomegaly
Muskuloskeletal- FROM but 2+ knee swelling, warm and 2+ tender to palpation.
DDX: Mono, CMV, Infectious, Hematologic(ALL, Lymphoma), Auto immune
Plan: CBC, CMP, Peripheral smear, ANA, anti DNA, CRP, RF
CBC results: 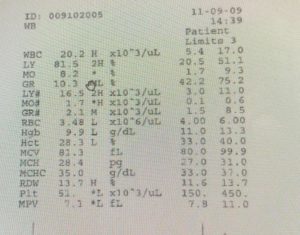
CBC result is more consistent with hematologic issue so patient was transferred to the emergency room to r/o ALL
February 13th, 2020
Presents with chills, fever (101.5), nasal congestion and headache. Vomiting X1 denies cough, chest pain, sore throat, night sweat, diarrhea, no shortness of breath. He had pneumonia in 2019,2018
The patient parents are worried about
PE- temp 103.5,
HEENT- 2+ nasal congestion (clear D/C) sinus non-tender to percussion
All other PE is remarkable
Flu Neg for A&B CBC: 7.2 WBC, 80%segs 14%lymps 6% mono
IMP- viral syndrome
Plan- supportive (temp control, fluids, rest), if other symptoms develop or symptoms get worse RCT to the clinic
February 14th, 2020
The patient returns the next day with right side chest pain, productive cough, greenish-yellow sputum, persistent soreness 4-5/10, no dyspnea, the movement does not make it worse,
DDx: lower respiratory tract (bronchitis/pneumonia), cardiac, pleuritis, pneumonia, embolism, muscular-skeletal


