Assignment: Pathophysiology of portal hypertension, sign and symptoms (clinical presentation) complication
Background on the Portal Venous system
The normal flow of blood:
The portal venous system drains the blood from the GI tracts via the splenic and mesenteric veins and removes the toxins before reaching the heart.
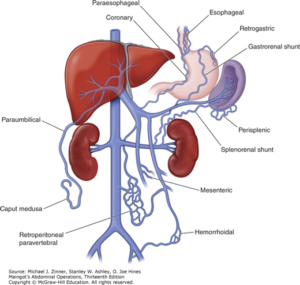
There are three points where the portal venous system connect with the systemic Venous system: the inferior portion of the esophagus, the superior portion of the anal canal, and the round ligament.
What is Portal Hypertension?
The portal and the systemic venous have less than 12 mmHg of pressure however if the pressure in the portal vein increases to >12 mmHg it can cause blood to shunt to the systemic venous system. The most common cause for raise in portal pressure is due to obstruction preventing blood flow from the portal vein to the IVC. The obstruction could be prehepatic, itra-hepatic or post hepatic. For our patient case chemotherapy could have caused intrahepatic damage which can create resistance to the passage of blood flow through the liver.
How Do Chemotherapy agents (MTX, asparaginase, cyclophosphamide) agent affect the liver
- hepatitis B and C (inflammation of the liver)
- nodules in the liver
- scarring of the liver (cirrhosis)
- hardening of the liver (fibrosis)
Symptoms and Signs [clinical Findings]
As the portal vein pressure increases and blood is stunting through the systemic venous system it can present as:
- Abdominal pain
- Portosystemic shunt causes the esophageal veins to enlarge or also known as esophageal varices that can present as gastrointestinal bleeding. Varices are very fragile and can easily rupture to cause a massive upper GI bleed.
- The vein in the anal canal can also enlarge and develop into hemorroids
- The round ligaments can rechannel the blood into the abdomen vein and present as caput Medusa
- Blood can back up into the spleen which can cause splenomegaly
- Endothelial cells release nitric oxide and cause atrial dilation which causes the BP to drop and stimulate the aldosterone system. As the kidney retains more water and sodium to elevate the BP it causes the plasma volume to expand so much that fluid from the vessel pushes into tissue like peritoneal cavity which causes Ascites
- Low-grade hepatic encephalopathy is common in patients with noncirrhotic portal vein thrombosis
Laboratory Tests
- Complete blood count may reveal thrombocytopenia and other findings of hypersplenism
- Liver chemistries are usually normal
- An underlying hypercoagulable state is found in many patients
Imaging
- Color Doppler ultrasonography and contrast-enhanced CT are usually the initial diagnostic tests for portal vein thrombosis.
- Magnetic resonance angiography (MRA) of the portal system is generally confirmatory.
- In patients with jaundice, magnetic resonance cholangiography may demonstrate compression of the bile duct by a large portal cavernoma (portal biliopathy)
- In patients with pylephlebitis, CT may demonstrate an intra-abdominal source of infection, thrombosis or gas in the portal venous system, or a hepatic abscess.
Other Studies
- Endoscopy shows esophageal or gastric varices.
- Needle biopsy of the liver may be indicated to diagnose schistosomiasis, nodular regenerative hyperplasia, and noncirrhotic portal fibrosis and may demonstrate sinusoidal dilatation.
- A low liver stiffness measurement by elastography may help distinguish noncirrhotic portal hypertension from cirrhosis
Primary complications of portal hypertension
- Gastroesophageal varices with hemorrhage
- Ascites
- Hypersplenism
- Hepatic encephalopathy
- Spontaneous bacterial peritonitis
- Hepatorenal syndrome
- Hepatocellular carcinoma
Sources:
- Harrison’s manual of Medicine- Portal Hypertension
- Current Medical Diagnosis and Treatment 2020
- Quick Medical Diagnosis & Treatment 2020
- Osmosis – https://www.youtube.com/watch?v=VTnAp-ngAXw
- https://www.youtube.com/watch?v=Cox6Z5pqMBo


